This post is by Richard Hassall, a qualified clinical psychologist, now retired. After retirement, Richard enrolled at the University of Sheffield to do an MA in philosophy, followed by a PhD which was completed in 2022. At the time of writing, Richard is an affiliate researcher attached to the Department of Philosophy at Sheffield.
 |
| Richard Hassall |
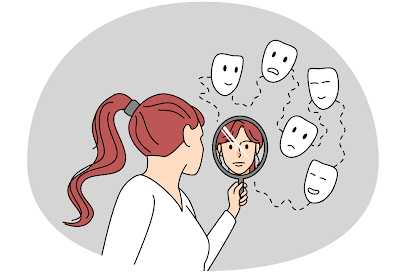
My area of interest is philosophy of psychiatry, with a particular interest in the nature of psychiatric diagnostic categories and the effect these have on the individuals who receive them. I argue in my PhD thesis that a psychiatric diagnosis may, in some cases, lead the recipient to becoming a victim of epistemic injustice, and specifically of hermeneutical injustice. I argue that this effect can be understood in terms of narrative theory and the self-narratives that individuals construct for themselves.
People gain meaning in their lives through their self-narratives, but such narratives can be changed by the person’s social circumstances and by extraneous events. Receiving a psychiatric diagnosis is one such event in some people’s lives, and it can significantly impact on the recipient’s self-narrative.
The codification of psychiatric diagnoses in disease nosologies, such as the DSM-5 of the American Psychiatric Association, can convey the implication that these represent disease entities of some sort. Patients are often told that their condition is “an illness like any other”. The reductionist methodology characteristic of the biomedical model of diseases can suggest that mental disorders are somehow caused by neurochemical abnormalities in the brain, an idea reinforced by the frequent treatment of such disorders with medication. Consequently, the diagnosis may be understood as a medicalized explanation of the person’s difficulties. However, most such diagnoses are based purely on symptom descriptions and do not explain how the person’s symptoms arose.
The medicalization implicit in psychiatric diagnoses conveys a biomedical narrative which may conflict with or marginalise the recipients’ previous self-narratives at a time when they will be experiencing significant emotional distress. As such, the recipients’ own hermeneutical resources can become marginalised. In other words, their capacity for understanding and expressing their own experiences can be minimised or neglected by clinicians. This can result in them becoming victims of hermeneutical injustice, particularly if they are mistakenly led to believe that their condition is a chronic one, from which full recovery is unlikely to happen.
The biomedical narrative associated with such diagnoses can undermine the recipients’ beliefs about their sense of agency and lead to feelings of hopelessness about recovery. While it is not an inevitable consequence of such diagnoses, there is evidence from testimonies of former service-users that this can happen to some people.
No comments:
Post a Comment
All comments are moderated.